Impacts of Expanding and Lowering a Cap on Out-of-Pocket Drug Costs
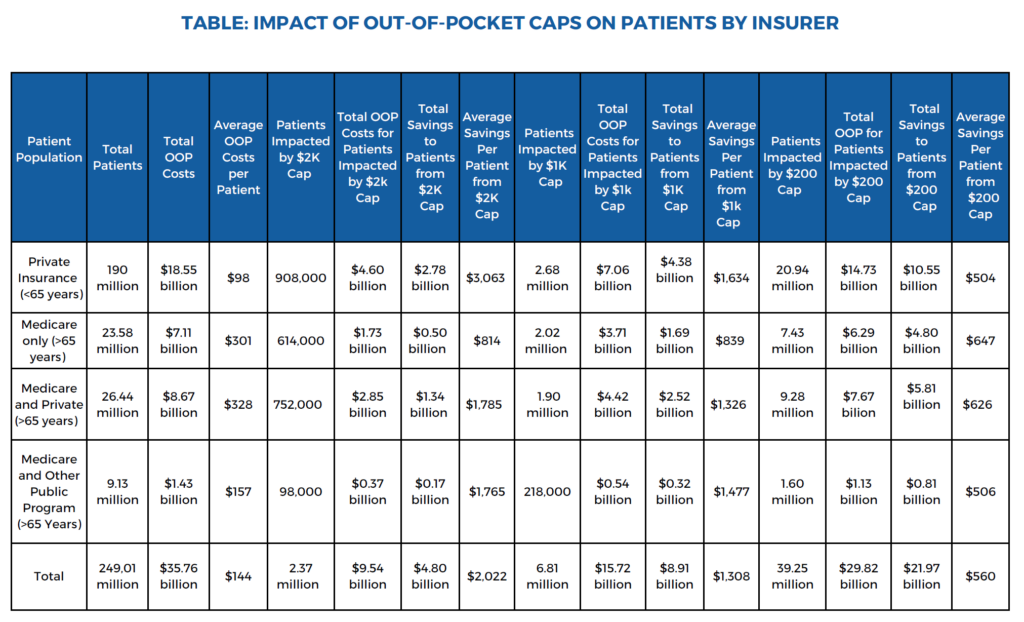
Impacts of Expanding and Lowering a Cap on Out-of-Pocket Drug Costs Table: Impact of Out-of-Pocket Caps on Patients by Insurer
The Inflation Reduction Act, signed into law by President Biden in August 2022, for the first time established an annual cap on out-of-pocket (OOP) costs for patients with Medicare Part D. Currently, Part D enrollees’ OOP costs are capped at about $3,500 per year. [i] On January 1, 2025, these drug pricing provisions will cap the OOP costs for prescription drugs across all Medicare plans at $2,000 per year, helping nearly 19 million seniors save about $400 annually. [ii]
The White House’s proposed FY2025 Budget and legislators have proposed extending the $2,000 OOP cost cap to patients with private insurance. Using data from the Medical Expenditure Panel Survey for 2022, research associates at Public Citizen estimated the potential impacts had such a policy been in place for Medicare and private insurance that year. Public Citizen also examined the potential impacts of lower annual OOP cost caps.
Key findings
- A $2,000 annual cap would have reached more than 900,000 patients with private insurance, saving them a total of $2.78 billion, equating to over $3,000 in savings per patient.
- A $1,000 annual cap would have reached nearly 2.7 million patients with private insurance and saved them a total of $4.38 billion, equating to over $1,600 in savings per patient.
- A $1,000 annual cap would have reached 4.1 million Medicare enrollees and saved them $4.53 billion in aggregate, saving each affected enrollee nearly $1,100 on average.
- A $200 annual cap would have reached nearly 21 million patients with private insurance and saved them a total of $10.55 billion, equating to over $500 per patient.
- A $200 annual cap would have reached more than 18 million Medicare enrollees and saved them a total of $11.42 billion in out-of-pocket costs, equating to over $600 per affected enrollee.
Discussion
Due to the high costs of prescription drugs, nearly a third of Americans do not take medications as prescribed. This includes cutting pills in half, skipping doses, not filling a prescription, or taking over-the-counter drugs instead of filling a prescription due to cost barriers. [iii] Data shows that about 5% of patients abandon their medications when they are free, but non-adherence increases to 60% when patients face out-of-pocket costs greater than $500 for a medication. [iv] Improved adherence to medications can help patients avoid poorer health outcomes, like increased risks of morbidity and mortality, as well as prevent increased health care service utilization. [v]
The imperative of lowering costs for patients to improve adherence and relieve financial stress is clear, but unless OOP cost caps are passed alongside policies to lower the prices drug corporations charge for medicines, they risk shifting costs onto other patients through higher premiums as well as other health care payers. The federal government could provide relief, but without reducing prices, taxpayers would be left on the hook.
Legislators must pass OOP cost protections and reforms to lower prescription drug prices together. Building on drug price negotiation and inflation rebates passed through the Inflation Reduction Act could help lower drug prices dramatically. For example, the Congressional Budget Office estimated that the Elijah E. Cummings Lower Drug Costs Now Act would lower spending by more than $450 billion over ten years, compared to the $101 billion in savings it projected for drug price reforms passed through the Inflation Reduction Act. [vi] That legislation, which was passed unanimously by House Democrats, went further than reforms included in the Inflation Reduction Act by using international reference pricing, increasing the number of drugs negotiated each year, expanding negotiation eligibility (including by allowing negotiations for expensive medicines without delay periods), and providing access to negotiated prices in private insurance.
Appendix: Methods
Data was obtained from the Medical Expenditure Panel Survey for 2022. Insurer type was based on full year insurance reported in the survey. For each insurance group we summed total out-of-pocket drug expenditures. We then tabulated how many individuals spent more out-of-pocket than each cap amount and summed their expenditures above the cap. To determine per-patient savings we divided total expenditures above the cap by the total number of persons whose expenditures exceeded the cap. [vii]
Endnotes
[i] Out-of-Pocket Cap Savings for Medicare Part D Enrollees, U.S. Dep’t Health & Human Servs., https://www.hhs.gov/inflation-reduction-act/outofpocketcap/index.html#:~:text=Thanks%20to%20the%20Biden%2DHarris,costs%20capped%20at%20about%20%243%2C500 (last visited Oct. 17, 2024).
[ii] FACT SHEET: President Biden Takes New Steps to Lower Prescription Drug and Health Care Costs, Expand Access to Health Care, and Protect Consumers, The White House (Mar. 6, 2024), https://www.whitehouse.gov/briefing-room/statements-releases/2024/03/06/fact-sheet-president-biden-takes-new-steps-to-lower-prescription-drug-and-health-care-costs-expand-access-to-health-care-and-protect-consumers/#:~:text=Expand%20Cap%20on%20Out%2Dof%2DPocket%20Prescription%20Drug%20Costs.&text=The%20President%20is%20calling%20on,putting%20food%20on%20the%20table.
[iii] Grace Sparks, Ashley Kirzinger, Alex Montero, Isabelle Valdes, & Liz Hamel, Public Opinion Prescription Drugs and Their Prices, KFF Polling (Oct. 4, 2023), https://www.kff.org/health-costs/poll-finding/public-opinion-on-prescription-drugs-and-their-prices/..
[iv] IQVIA, Medicine Spending and Affordability in the U.S. (Aug. 4, 2020), https://www.iqvia.com/insights/the-iqvia-institute/reports-and-publications/reports/medicine-spending-and-affordability-in-the-us.
[v] Marie T. Brown, Jennifer Bussell, Suparna Dutta, Katherine Davis, Shelby Strong, & Suja Mathew, Medication Adherence: Truth and Consequences, 351 Am. J. Med. Sci. 387 (2016).
[v] IQVIA, Medicine Spending and Affordability in the U.S. (Aug. 4, 2020), https://www.iqvia.com/insights/the-iqvia-institute/reports-and-publications/reports/medicine-spending-and-affordability-in-the-us.
[vi] Compare Letter from Phillip L. Swagel, Director, Con. Budget Off., to Honorable Frank Pallone Jr., Chairman, Comm. Energy & Commerce, U.S. House of Reps., Budgetary Effects of H.R. 3, the Elijah E. Cummings Lower Drug Costs Now Act, https://www.cbo.gov/system/files/2019-12/hr3_complete.pdf, to Cong. Budget Off., Estimated Budgetary Effects of Subtitle I of Reconciliation Recommendations for Prescription Drug Legislation, as Posted by the Senate Committee on Finance on July 6, 2022, https://www.cbo.gov/system/files?file=2022-07/senSubtitle1_Finance.pdf (last visited Oct. 17, 2024).
[vii] Our estimates differ in important ways from those included in a recent HHS report. See Assistant Sec. Planning & Evaluation, Off. Health Pol’y, Medicare Part D Enrollees Reaching the Out-of-Pocket Limit by June 2024 (Oct. 22, 2024). To assess Medicare Part D enrollees reaching drug expenditures thresholds in 2024, that report counted government expenditures for enrollees in the Low Income Subsidy program, as well as out-of-pocket spending, while our analysis only assessed enrollees’ actual out-of-pocket spending. Additionally, our estimates were based on a survey that did not include patients in nursing homes and other institutional setting (who likely incur high out-of-pocket costs). We also excluded from our table Medicare enrollees below the age of 65 because there were only 165 respondents who fit inclusion criteria for this group. However, the data suggested aggregate out-of-pocket spending for this group would be approximately $810 million which does not significantly affect our estimates. Finally, we used data from 2022, without accounting for increases in drug costs since then.